Sciatica is like that one group chat notification that keeps popping up at the worst time. It’s that nerve trouble that decides to ride the sciatic nerve with shocks, tingles, and jolting leg pain that hits different.
However, let’s be real, this isn’t some random BUMMER. It’s your body throwing a signal that something deeper is off in the lower back region. Once you understand what it’s saying, you can address the root cause instead of living with the chaos.
What Exactly Is Sciatica? (And What It Isn’t)
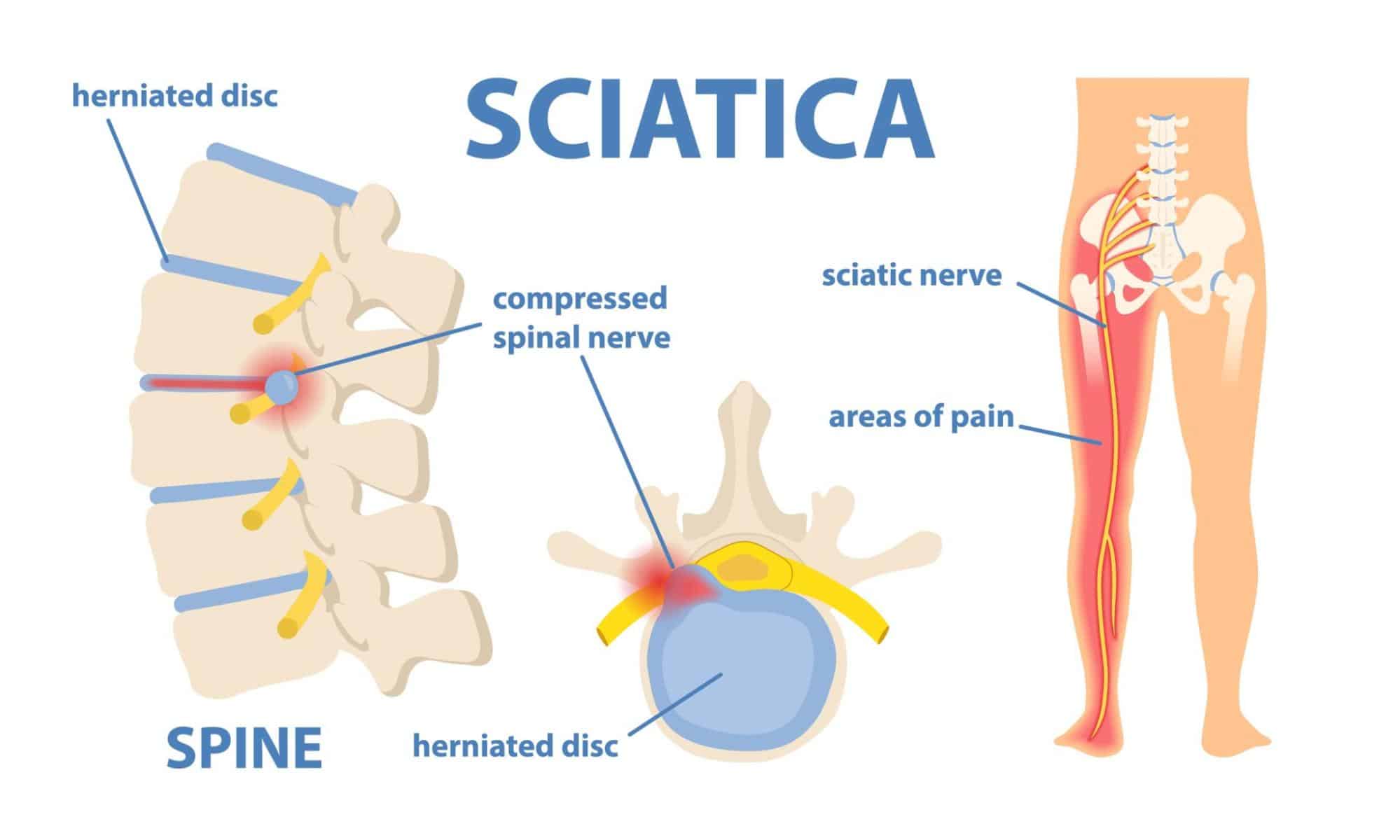
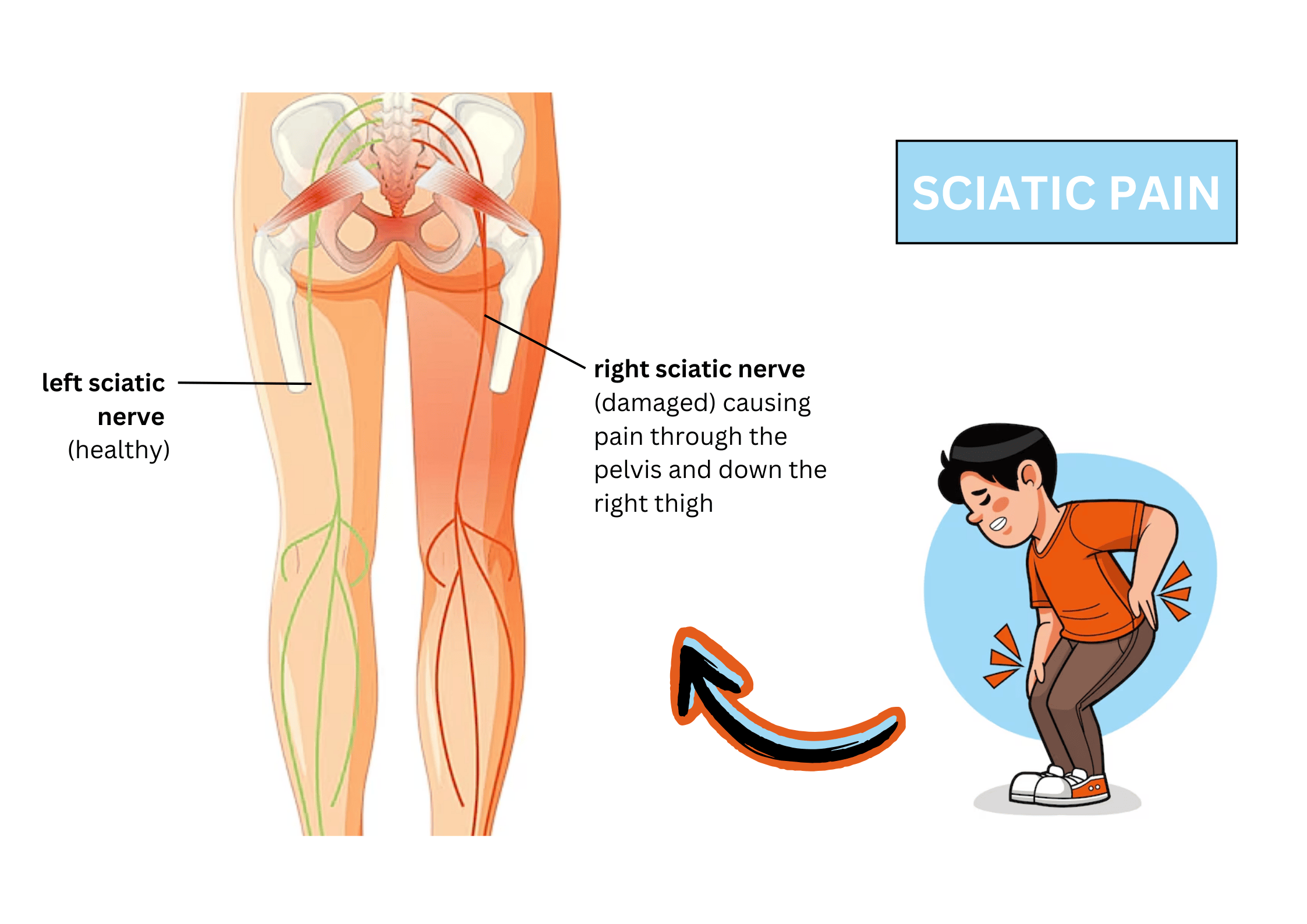
First things first, this pain isn’t some mystery monster. Sciatica occurs when your lumbar nerve roots become irritated or compressed. This pressure fires up the sciatic nerve, the GOAT of nerves. It’s the biggest, longest nerve in the body, running from the lumbar spine through your hips and all the way down each leg.
Think of it like a highway. When traffic flows smooth, signals cruise without issue. When there’s a roadblock like a bulging disc or bone spur, everything jams up. The result: burning, tingling, or straight-up radiating leg pain. It’s a clear sign something’s off, and the smart move is to understand what’s causing that compression.
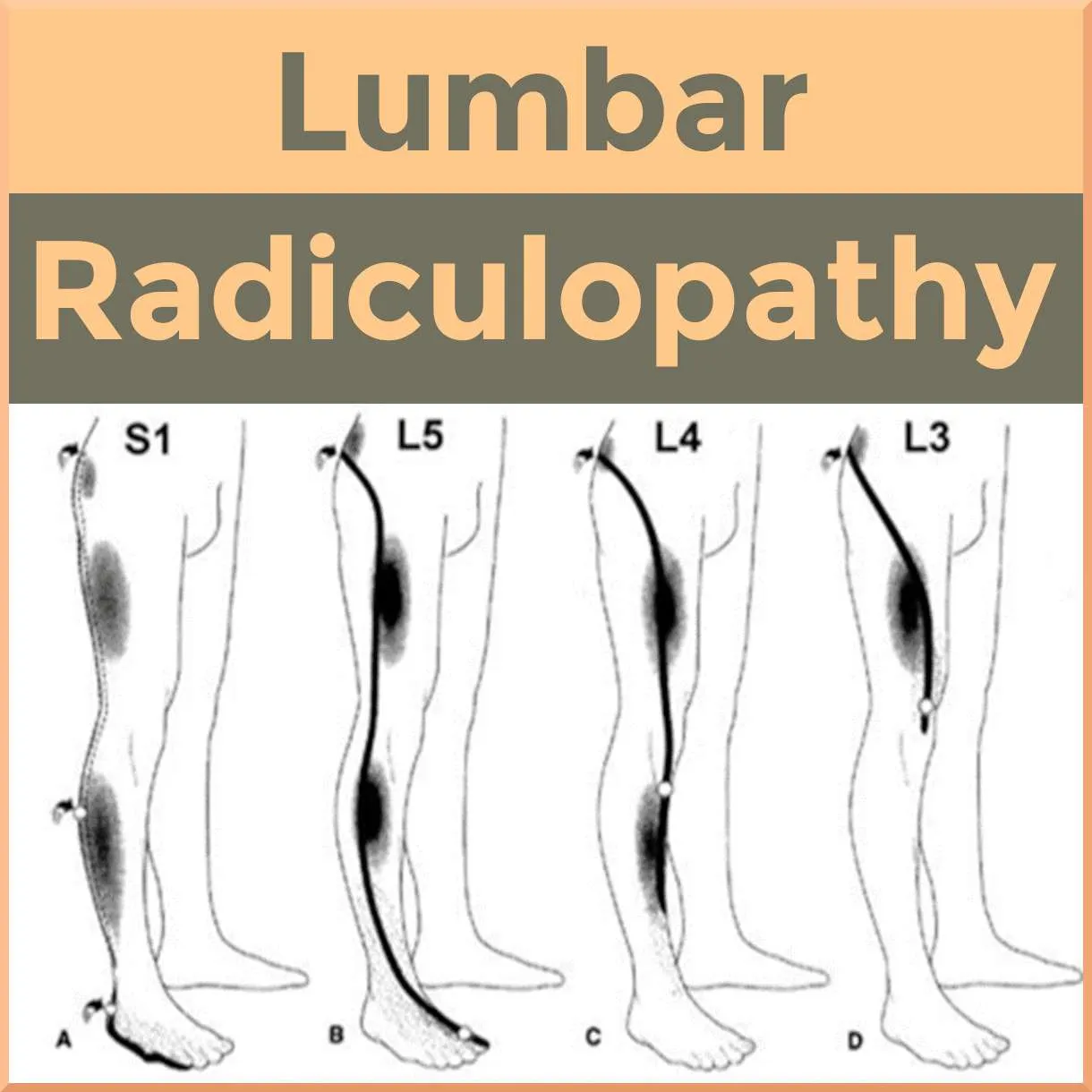
Now, don’t get it twisted. People often confuse lumbar radiculopathy, piriformis syndrome, and deep gluteal syndrome with Sciatica. Lumbar radiculopathy is the umbrella term for any irritation of spinal nerve roots. Piriformis syndrome and deep gluteal syndrome are muscle problems, where a tight hip muscle presses on the nerve. Sciatica is different — it’s nerve root irritation right at the spine.
Lumbar Radiculopathy
Piriformis vs True Sciatica
| Feature | Piriformis Syndrome | Sciatica (True) |
| Cause | Piriformis muscle squeezes the nerve | Irritation in nerve root in the spine |
| Symptoms | Buttock pain, worse with long sitting | Shooting leg pain, tingling, weakness |
| Area Hit | Hip + buttock mostly | Back down the leg into the foot |
| Fix Focus | Piriformis stretch, posture for sciatica | Rehab, decompression, leg nerve glide |
Spot the Signs: Common Symptoms of Sciatica
This pain doesn’t play nice. It typically presents as sharp leg pain on one side, sharp enough to stop you mid-step. Add in glute pain, hip aches that spread, or that “pins-and-needles” vibe called leg numbness and tingling. Some people even get foot/leg weakness, like their muscles ghosted them.
Here are the symptoms that are totally a sign your nerve is not okay.
| Symptom | Description |
| Pain | A burning or electric shock sensation that shoots down one leg. It can be a real jump scare when you cough, sneeze, or bend over. |
| Tingling | That “pins and needles” feeling, like your leg fell asleep and is now trying to wake up. It’s low-key a chaotic feeling. |
| Numbness | A lack of sensation. You can’t feel things on your leg or foot because the signals are not getting through. |
| Muscle Weakness | Your muscles feel weaker because the command signals from your brain are getting lost. It’s a more serious symptom. |
| Loss of Control | A very severe symptom. If you suddenly lose control of your bladder or bowels, it’s a huge red flag, and you should seek medical attention ASAP. |
At a Glance of Common Symptoms vs Red Flags
| Vibe Check | Symptoms |
| Everyday Signs | Shooting leg pain, glute pain, leg numbness and tingling, foot/leg weakness |
| Cauda equina red flags | bladder/bowel changes, saddle numbness, worsening weakness |
The Top Causes of Sciatica
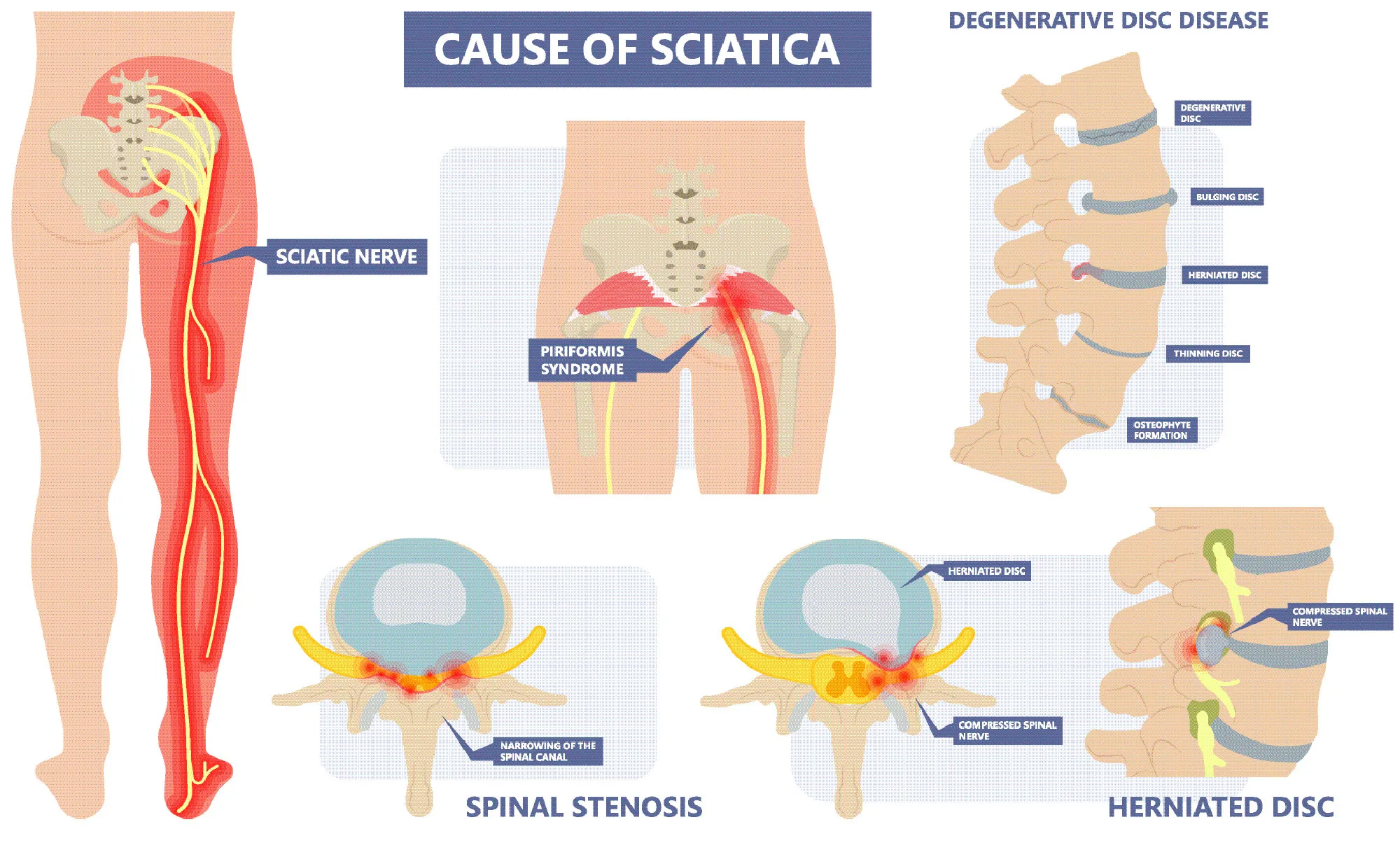
Here are the main villains — each with their own way of messing with your nerve.
-
Herniated disc
Picture your spinal discs like jelly-filled donuts. Most of the time, they cushion your vertebrae like champs. Stay slouched too long, though, and the jelly bulges out. That bulge can press on a nerve root, causing instant drama — the kind of nerve compression that sends pain shooting down your leg.
-
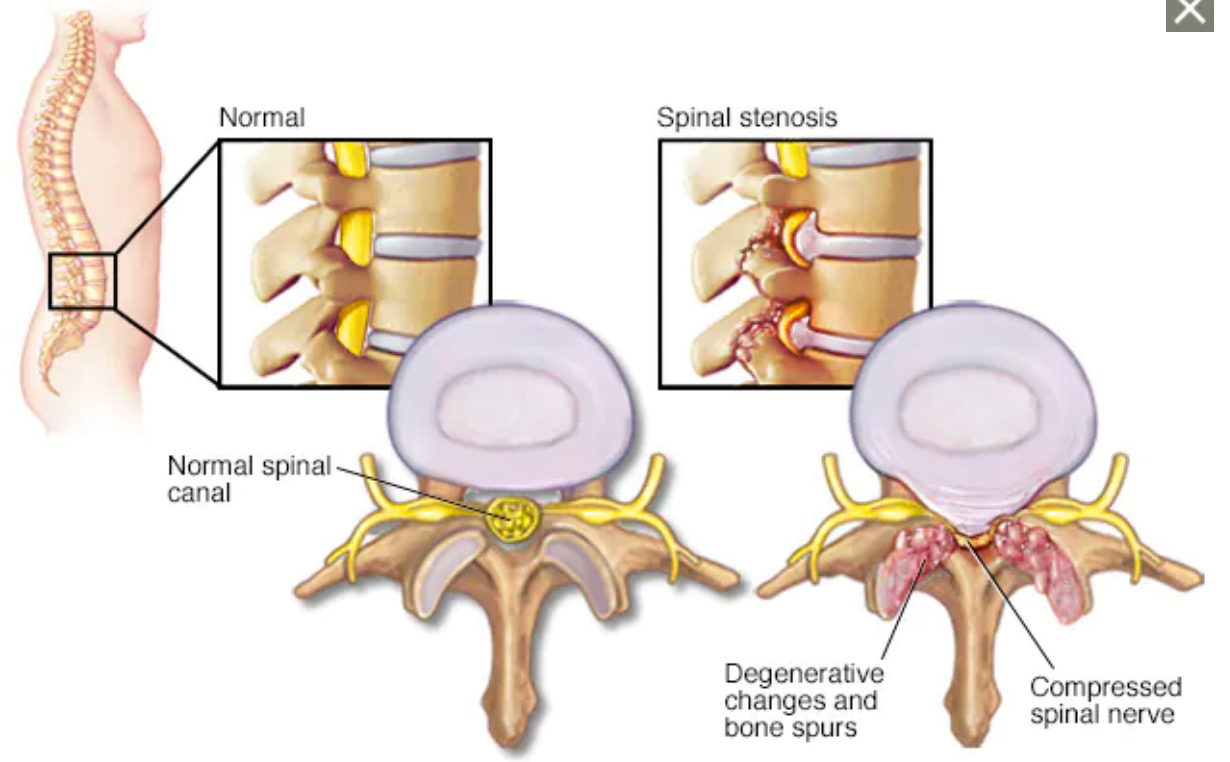
Spinal stenosis
This one’s like your spinal canal going on a slow shrink mode. The space where your nerves should glide gets crowded. Aging, injuries, or extra weight can make the canal smaller, leaving the sciatic nerve feeling cornered. Cue the pain.
-
Spondylolisthesis
Here, one vertebra slides forward over another. Think of it like a block slipping out of a stack. That slip crowds the nerve’s exit, leaving it trapped.
-
Piriformis syndrome
Not always about the spine. A tight piriformis muscle in the hip can squeeze the nerve root like a clamp, resulting in sharp buttock pain and leg irritation that mimics spinal sciatica.
-
Kinetic chain chaos
Your body works as one linked system. Uneven hips, tight hip flexors, or poor posture throw off the pelvis. That tilt stacks stress on the lower back area, setting the nerve up for irritation.
Risk Factors That Increase Likelihood
Sometimes it’s not just the root cause — it’s the lifestyle vibes that make sciatic nerve flare harder. Here are the main risk factors that put the nerve on edge:
- Age 30–50 —> Most people first meet Sciatica in this window. Discs are more likely to wear down, and injuries stack up. It’s prime time for nerve trouble to sneak in.
- Sedentary lifestyle/desk jobs —> Prolonged sitting (especially slouched at a desk or on a long car ride) loads pressure straight onto the nerve. Hours of no movement = fast-track to irritation.
- Obesity and diabetes —> Extra body weight keeps the spine under stress 24/7, while diabetes sparks nerve inflammation. Together, they create the perfect storm for flare-ups.
- Heavy lifting, twisting jobs —> Lifting with bad form or constant twisting overloads the discs. It’s basically inviting a bulging disc to show up and press on the nerve.
- Poor posture, weak core muscles —> A weak core means less protection for the spinal support. Pair that with poor posture, and the sciatic nerve gets zero backup.
- Pregnancy (pressure on spine) —> Relaxed ligaments + shifting weight load = more strain on the lower back. That extra pelvic pressure can irritate the nerve until delivery day.
Diagnosis: How Doctors Confirm Sciatica
Confirming this symptom is all about connecting the dots. Doctors use a mix of questions, physical checks, and sometimes imaging to figure out what’s really irritating the nerve.
-
History first
Your story matters. When the pain started, how far it travels, and what makes it worse or better all give clues. Even lifestyle habits like long sitting or heavy lifting can help pinpoint the cause.
-
Walking assessment
A change in the way you move often reveals nerve issues. If your stride is uneven or guarded, it can signal nerve compression along the pathway of the nerve root.
- Straight-leg raise test
This one is a classic. You lie on your back, the doctor slowly lifts your leg, and if that familiar electric shock pain fires down, it suggests the irritation in the nerve root is in play.
-
Reflex and muscle strength checks
Weak ankles, reduced knee reflexes, or trouble pushing against resistance show that the nerve irritation isn’t just causing pain — it’s affecting strength and coordination too.
-
Imaging: MRI or CT scan
If symptoms are severe, persistent, an MRI is usually the go-to because it shows the soft tissues clearly. It can highlight a herniated disc, spinal stenosis, or other issues that squeeze the nerve. CT scans are sometimes used to spot bone changes like arthritis or spondylolisthesis.
Think of diagnosis like detective work. Each test adds a piece of the puzzle, until the exact source of the pain is revealed. That’s how a treatment plan gets targeted instead of random.
How Sciatica Affects Daily Life (Beyond Pain)
It isn’t just about pain — it’s about how that pain sneaks into every corner of your routine.
- Sitting, driving, desk work
Long hours in a chair become uncomfortable fast. Sitting in traffic or at a desk adds pressure on the sciatic nerve, so what used to be routine suddenly feels like a challenge. Even adjusting posture doesn’t always give instant relief, which makes workdays and commutes tougher.
- Sleep disruption
Lying down should be the reset button, but Sciatic pain often makes it complicated. Certain positions trigger tingling or hip discomfort, forcing people to toss and turn. Poor sleep then adds fatigue on top of the nerve irritation, creating a cycle of low energy and higher discomfort.
- Emotional health
Chronic nerve pain chips away at patience. The frustration of not being able to sit comfortably, go for a walk, or even sleep well can build up. Many people worry about their future, with thoughts like “Will I need surgery?” or “Will this ever end?” That fear often feels heavier than the pain itself.
- Why ignoring it backfires
Hoping it will just disappear isn’t the best move. If left untreated, the pain can turn from an occasional flare-up into a chronic condition. Ongoing nerve compression can lead to weakness, reduced mobility, and even long-term changes in how the body moves. Addressing it early means better outcomes, less frustration, and fewer long-term issues.
8. Relief You Can Start Today (Step-by-Step Guide)
Phase 1: First 48–72 Hours (Acute Phase)
Goal = cool it down, don’t fire it up.
- Ice first → 10–20 minutes at a time, a few cycles per day. Keeps swelling low and numbs the sting.
- Pain-free positions → Lying on your back with knees propped on a chair gives instant pressure relief.
- Gentle sciatic nerve glide → Small, slow leg movements to keep the nerve moving without stretching it too far.
- Avoid aggressive stretching — now’s not the time.
Phase 2: After Inflammation Calms (Sub-acute Phase)
Once the sharp sting eases a bit, it’s time to loosen muscles and start gentle strengthening.
- Switch to heat
Use a heating pad or warm towel for 10–20 minutes. Warmth relaxes stiff muscles and helps blood flow, so the area feels less tight. - Piriformis Stretch (Figure-4)
Lie on your back. Cross your right ankle over your left knee so it looks like a “4.” Grab behind your left thigh and pull toward your chest. You’ll feel a stretch in your hip and butt. Hold 20–30 seconds. Do 2–3 rounds on each side. - Pelvic Tilts
Lie on your back with knees bent. Flatten your lower back into the floor by gently tightening your abs, then release. This strengthens the small stabilizer muscles in your core. Do 10 reps. - Supine Leg Over
Lie on your back. Bend one knee and gently cross it over your body, aiming for the floor. Keep shoulders flat on the ground. This opens up the lower back. Hold 30 seconds, repeat each side. - Bridge Exercise
Lie on your back, knees bent, feet on the floor. Slowly lift your hips up while squeezing your glutes, then lower back down. This strengthens your butt and back muscles to support your spine. Aim for 10–12 reps. - Bird-Dog Exercise
Start on hands and knees. Stretch your right arm forward and left leg back, hold 2–3 seconds, then switch sides. This move builds balance and stability in your core. Do 8–10 reps.
Think of Phase 2 like “rehab lite.” Warm the muscles, stretch gently, then add small strength moves to keep the nerve from flaring again.
9. Lifestyle & Ergonomic Fixes
Relief from the lumbar part isn’t just about exercises. Daily habits matter too, like the way you sit, sleep, and move can either calm the nerves or fire it up. Here’s how to stack the odds in your favor:
-
Workstation setup
The best sitting position for lumbar area is upright, not slouched. Use an ergonomic chair/lumbar support or place a cushion behind your back. Keep the screen at eye level to avoid hunching, and rest both feet flat on the floor. This posture takes pressure off the lower back area.
-
Driving smarter
Long drives load the lower back. A small lumbar roll or rolled towel helps, plus taking breaks every 30–40 minutes to stretch or walk resets the nerve. Think of it as a pit stop for your spine.
-
Better sleep positions
The goal with sleeping with sciatica is spinal alignment. Lying on your side with a pillow between your knees works wonders. Back sleepers can place a pillow under their knees to support their spine. Skip stomach sleeping — it twists the back and irritates the nerve.
-
Footwear check
Your shoes affect everything above them. Worn-out sneakers throw off alignment, while supportive footwear or orthotics help the body stack properly. Balanced feet = balanced hips and less nerve stress.
Prevention & Long-Term Management
The best move against radicular pain is stopping it from taking over long-term. Prevention isn’t fancy — it’s about consistent habits that keep your spine supported and nerves calm.
-
Maintain a healthy weight
Extra pounds mean extra load on the spine. Keeping weight in check reduces the pressure on discs and lowers the chance of pinched nerve sneaking back in.
-
Core + back strength
A strong core = natural armor for your lumbar spine. Simple moves like bridges, bird-dog, or planks train the muscles that stabilize and protect your back every day.
Three simple moves can make a huge difference:
- Bridges → Lie on your back, knees bent, feet flat. Lift hips into a straight line, squeeze glutes, lower down. Builds glute + lower back strength.
- Bird-Dog → On all fours, reach opposite arm + leg out, hold a few seconds, switch sides. Trains balance and keeps your core steady.
- Planks → On elbows and toes, hold your body in a straight line. Engages abs and spine-support muscles for full-core stability.
-
Ditch long sitting marathons
Hours in one chair set the stage for flare-ups. Break it up — stand, stretch, or walk every 30–40 minutes. Even a few steps count.
-
Follow an anti-inflammatory lifestyle
What you eat, drink, and smoke (or don’t smoke) all matter. A diet rich in colorful fruits, veggies, lean proteins, and healthy fats can calm body-wide inflammation. Pair it with no smoking and less alcohol, and you’ve got a setup that helps nerves recover faster and stay calmer over time.
When to See a Professional (And What to Expect)
Sometimes nerve pain chills out on its own. Other times it overstays its welcome. That’s when it’s time to tag in the pros.
-
When to go
If the pain drags on past 4–6 weeks, don’t wait it out. Big red flags like bladder changes, saddle numbness, or sudden leg weakness mean your time to get checked fast.
-
What happens at the clinic
Day one is simple: reflex checks, strength tests, maybe watching how you walk. If the nerve still isn’t backing down, scans like an MRI can show exactly where the nerve root irritation is coming from. First line of attack = conservative care.
-
Treatment options
-
-
- Physical therapy for sciatica → exercises and mobility work that take pressure off the nerve.
- Chiropractic care for sciatica → adjustments that realign things and give your back more freedom.
- Lumbar decompression therapy → gentle traction that literally makes space for the sciatic nerve.
- Pain management → tools to keep symptoms under control while healing.
- Injections or surgery → rare, last-card moves if nothing else works.
-
-
Timeline for results
Relief doesn’t take forever. A steady plan — 2–3 sessions a week of physio or chiro for about 4–6 weeks — usually brings solid improvement.
How Atlas Spine Clinic Can Help You Find Relief
At Atlas Spine Clinic, we know quick fixes don’t cut it. Our goal is to give you lasting relief with care that really works.
- Evidence-based care → Every plan is grounded in proven methods that actually work.
- Exercise rehab → Programs include moves like a bridge exercise or bird-dog exercise to build strength and take pressure off irritated nerves.
- Ergonomics coaching → Real-world tweaks for sitting, driving, and sleeping with sciatica, so your daily routine stops fueling the pain.
Atlas is trusted locally — patients share how they went from restless nights to full workdays or pain-free walks again. That community proof makes our care feel less clinical, more personal.
📞 Call us at (647) 794-6868 or
🖥️ fill out our online form to book an appointment or learn more about our services.
FAQs (Long-Tail Queries → Featured Snippets)
Q: What is the fastest way to relieve sciatica pain?
A: Use heat vs ice for sciatica. Ice during the first 48–72 hours helps calm inflammation, then switch to heat to relax tight muscles. Pair it with easy stretches like a piriformis stretch or pelvic tilts.
Q: Is walking good or bad for sciatica?
A: Walking usually helps. It keeps blood flowing and prevents stiffness. Just pace yourself, avoid rough ground, and pause if pain suddenly spikes.
Q: How long does sciatica usually last?
A: Acute cases can fade in a few weeks. Chronic ones may take longer, but sticking to consistent care and an anti-inflammatory lifestyle — balanced diet, regular movement, no smoking — shortens recovery time.
Q: Can sciatica heal without surgery?
A: Yes. Most cases improve with conservative care like physical therapy, chiropractic adjustments, and strengthening moves such as a bridge exercise or bird-dog exercise. Surgery is only a rare, last-resort option.
Q: Can sciatica cause permanent nerve damage?
A: It’s rare, but ignoring symptoms for too long can lead to lasting weakness or numbness. Spotting red flags early and seeking help keeps that risk low.