Knees pulling that inward swerve like they’re on autopilot? That’s knees caving in the classic knee collapse move also known as valgus alignment. It’s a very common issue, whether you’re squatting in the gym or just walking around.
The thing is, this inward cave-in doesn’t have to be your story forever. Fixing knee valgus means stronger hips, better balance, and way less pressure on your joints. By the end of this guide, you’ll know exactly what causes it and how to get your knees tracking straight again.
What Exactly Is Knee Valgus? (And What It Isn’t)
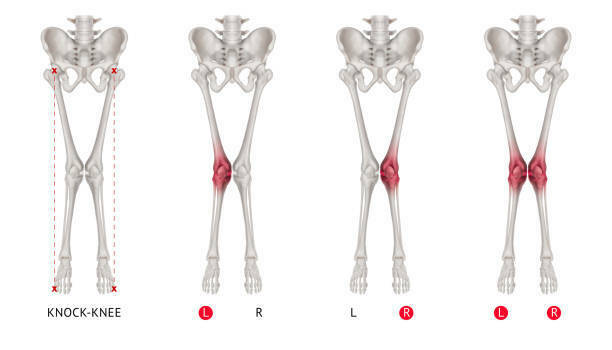
There’s more than one type of inward knee collapse, and mixing them up only creates confusion. The everyday version most people deal with in the gym is called dynamic valgus. This shows up when you squat, lunge, or land a jump, and it happens because of muscle control issues. The other term, genu valgum, refers to a structural condition, often called “knock knees,” where the bone alignment itself creates the inward angle.
Image Sources: Dynamic Valgus, Genu valgum
📊 Biomechanics Breakdown
Here’s what’s happening under the hood:
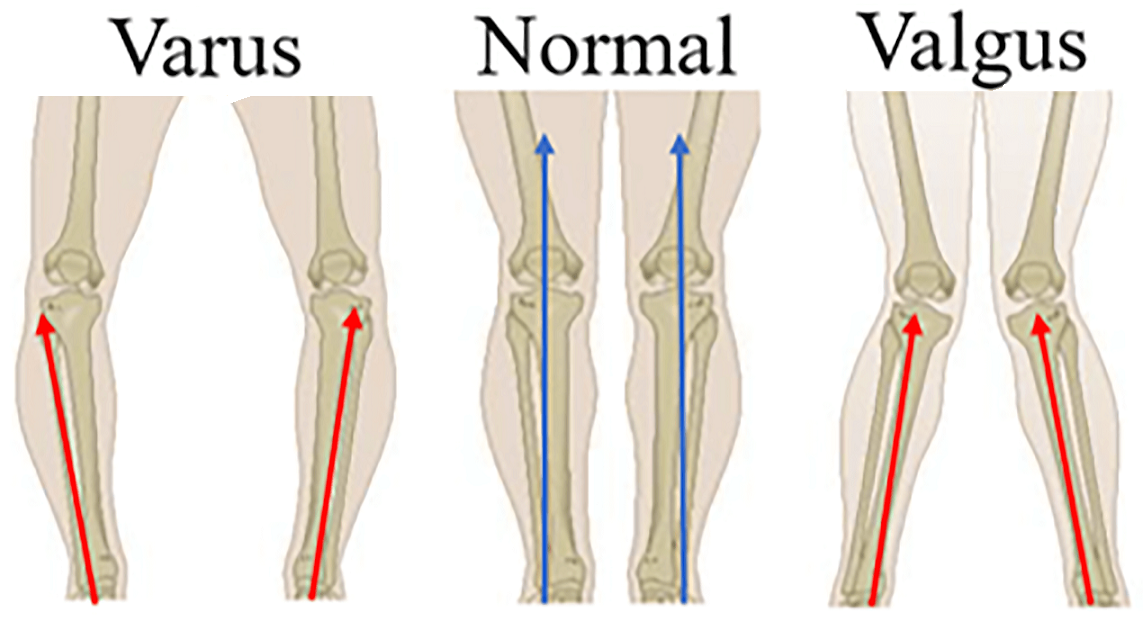
- The image shows that the femur drifts into femoral internal rotation, pulling the thigh bone inward.
- The shin responds with tibial rotation, twisting the lower leg and shifting load to the outside of the knee.
- This creates a larger Q-angle, meaning the kneecap tracks sideways instead of cleanly forward.
Image: Different types of Q-angle
These shifts throw the knee off its center line, forcing the patella to drift and creating instability. Over time, that movement pattern strains both cartilage and ligaments.
📚 Extra Support
Dynamic valgus is often linked with broader postural issues like hip weakness and pelvic tilt. For deeper reading on how this connects to the whole lower body, check out our guides on sciatica and uneven hips.
Biomechanics: Why Knee Valgus Matters
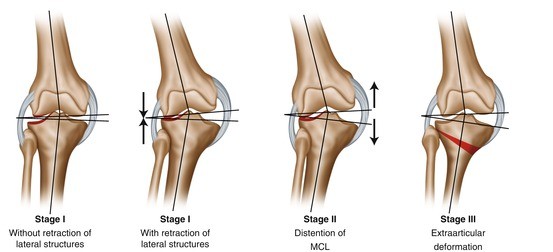
Flat feet, stiff ankles, lazy hips it all stacks up. Your body runs like a chain, so when one link slips, the others struggle. That’s why a dropped arch in your foot or weak glutes in your hip can end up showing as knee valgus.
Image: Patellofemoral imbalance creates joint surface wear.
Now for the science: when the knees cave in, the patellofemoral joint gets overloaded. A bigger Q-angle means your kneecap no longer tracks straight; it drifts sideways. That shift messes with joint loading, piling stress onto one side of the knee while the other side overstretches. Over time, that imbalance creates cartilage stress, which is basically wear-and-tear at the surface that cushions your joint.
Researchers put numbers behind it. A large cohort study in the Annals of the Rheumatic Diseases found valgus alignment made lateral knee osteoarthritis nearly five times more likely to progress (ScienceDirect, 2010).
So here’s the takeaway: what starts as a foot or hip issue snowballs into knee breakdown. The longer the chain stays out of sync, the more pressure builds until pain and long-term joint damage set in.
Signs & Symptoms of Knee Valgus
Your body doesn’t stay quiet when this symptom shows up. It drops hints all over.
- Uneven gait: Think wobbly walk, where one knee dives in more than the other. That off-beat stride is a dead giveaway that something’s misfiring.
Image: Uneven Gait
- Patellofemoral pain: A dull ache behind the kneecap or sharp twinges when squatting, climbing stairs, or sitting too long. This happens because the patellofemoral joint is tracking off-center, rubbing where it shouldn’t.
Image: The red part shows the inflammation & which caused pain
- Hip strain: Since weak glutes often start the chain reaction, your hips try to overcompensate. Result = constant tightness or fatigue up top.
- ACL risk: Athletes take note. That inward collapse puts nasty rotational forces on the anterior cruciate ligament. It’s the kind of silent setup that can tear an ACL in a split-second cut or jump.
👉 Red flag callout: If pain keeps escalating, you notice swelling, or your knee actually gives out during movement, that’s not a “walk it off” moment. It’s time to see a pro.
At Atlas Spine Clinic’s physiotherapy services, these exact signs are common. With guided rehab, patients regain stable movement, reduce pain, and protect their joints from long-term breakdown.
Why Do Knees Cave In? Root Causes
Knee collapsing isn’t one single problem. It’s a combo platter of weak hips, stiff ankles, flat feet, and unstable trunk control, all feeding into each other. Let’s break it down.
Foot & Ankle Causes
When the base collapses, the chain above crumbles. Foot pronation (the arch rolling inward) twists the tibia and drags the knee into collapse. Add limited ankle dorsiflexion (ankle flexion range), and the body cheats by letting the knees cave in just to reach depth in squats or lunges. This is why supportive footwear and custom orthotics matter check our Orthotics service page.
Hip & Glute Weakness
Hips are the gatekeepers of knee alignment. With hip abductor weakness, especially in the glute medius/maximus, the femur rotates inward unchecked. This is one of the most common culprits behind that “knees touching, ankles apart” look.
Core Dysfunction
Even strong legs can’t compensate for a weak center. Poor lumbo-pelvic stability throws off the kinetic chain, letting the hips wobble and the knees collapse. It’s a classic motor control issue: the brain and muscles aren’t syncing properly to hold alignment.
Quick Comparison Table:
| Cause | Effect on Knee | Fix Approach |
| Foot pronation | Pulls tibia inward → knee caves in | Supportive shoes, orthotics |
| Limited ankle dorsiflexion | Knee compensates by collapsing inward during squats | Mobility drills, ankle stretches |
| Hip abductor weakness | Femur rotates inward, no control at the thigh | Glute medius/maximus strengthening |
| Core dysfunction (poor motor control) | Pelvis unstable → hips/knees fall out of alignment | Core stability + neuromuscular retraining |
Knee valgus is rarely just about the knee. It’s usually the ripple effect of weak links across the chain. Strengthen the hips, free the ankles, support the feet, and stabilize the core that’s how you stop the collapse.
Risk Factors That Make Knees Cave In Worse
Not everyone is equally at risk. Certain factors make inward collapse more likely and harder to control.
- Female athletes → Women tend to have a naturally wider pelvis, which increases inward pull at the knees. Pair that with high-impact sports like soccer, basketball, or volleyball that demand constant cutting and jumping, and the chance of misalignment climbs fast.
- Obesity → Extra body weight multiplies the load through every step. That added pressure forces joints to absorb more stress than they’re built for, speeding up the collapse.
- Repetitive sports → Activities that hammer the same motion repeatedly, like long-distance running or heavy squat programs, gradually wear down stabilizers. Without recovery, the knees eventually give in under the strain.
- Sitting lifestyle → Long hours at a desk weaken glutes and tighten hip flexors. This destabilizes the pelvis and removes the critical support system needed for proper knee alignment.
These risk factors don’t guarantee collapse, but they tilt the odds against you. Building strength and fixing lifestyle triggers can help.
How to Assess Yourself at Home
Quick DIY checks can reveal if your knees are drifting inward. Try these at-home tests:
| Test | How to Do It | What It Shows |
| Mirror Squat | Stand in front of a mirror and perform a bodyweight squat. | Knees should track over feet inward drift = collapse |
| Single-Leg Squat | Balance on one leg, squat down slowly, and watch for wobbling. | Knee wobble or hip drop = weak stabilizers |
| Knee-to-Wall Test | Place foot a few inches from a wall, tap knee forward without lifting the heel. | Limited reach = ankle mobility restriction |
| Video Analysis | Record squats, lunges, or jumps in slow motion on your phone. | Highlights subtle inward shifts or pelvic tilt |
The Consequences of Ignoring It
Letting the knees keep caving inward isn’t harmless. Over time, that small inward shift stacks up into bigger conditions that affect mobility, comfort, and long-term joint health. Here’s what’s really at risk:
Runner’s Knee (Patellofemoral Pain Syndrome)
What it is: Runner’s knee is a broad term that describes pain around the kneecap, especially during repetitive activities like running, squatting, or stair climbing. This condition happens when the patella (kneecap) doesn’t sit properly in the groove of the femur (thigh bone).
Why it matters: When the knee tracks poorly, the kneecap doesn’t glide smoothly over the thigh bone. That uneven motion irritates the joint and surrounding tissues, leaving you with aching or burning pain at the front of the knee. If ignored, it can limit basic activities, not just sports.
Osteoarthritis
What it is: It is the gradual wearing away of cartilage the protective cushion inside joints.
Why it matters: When inward collapse shifts body weight unevenly, one side of the joint absorbs more stress. Over years, this overload erodes cartilage faster, leading to stiffness, swelling, and loss of mobility. Unlike sore muscles, cartilage damage doesn’t heal on its own, which is why prevention and correction are critical.
ACL Tear
What it is: The Anterior Cruciate Ligament (ACL) is one of four major ligaments in the knee. Running diagonally through the joint, it connects the femur (thighbone) to the tibia (shinbone) and plays a crucial role in stabilizing the knee during quick pivots, stops, and landings.
Why it matters: Inward collapse puts rotational stress on the ACL. One bad landing or sudden twist can push it past its limit, causing a tear. This injury is infamous among athletes for its severity usually requiring surgery, followed by months of rehab to rebuild stability and strength.
When these risks stack up, the damage isn’t limited to the knees. Compensation often spread to the hips and lower back, creating even more pain down the line. That’s why early action is key check out our back pain content to see how these issues connect across the body.
Step-by-Step Fixes for Knee Valgus
Knees caving in don’t need to be your permanent vibe. With the right moves, you can rebuild alignment, unlock power, and finally shut down knee valgus for good. Here’s the playbook:
1. Activation: Wake Up the Right Muscles
Most people with inward collapse have lazy hip stabilizers. If the gluteus medius isn’t firing, the femur rotates inward and the knees drift. Activation drills “switch on” these muscles so they actually do their job.
- Isometric holds → Lie on your back, squeeze your glutes hard, and hold for 20–30 seconds. This builds awareness of proper hip engagement.
- Banded glute bridges → Place a resistance band just above your knees, push outward as you lift your hips. The band forces the glutes to kick in, training you to keep knees from caving.
2. Strength: Build Stability That Lasts
Once muscles are awake, it’s time to strengthen them so they can support you under pressure. Weak hips and poor pelvic control are the top drivers of inward knee collapse.
- Clamshells → Lying on your side, lift your top knee while keeping feet together. This directly targets the gluteus medius, the muscle that fights collapse.
- Monster walks → With a band around your knees or ankles, take controlled side steps. The constant outward push builds hip endurance and trains better alignment.
- Hip hitches → Stand on a step with one foot, let the opposite hip drop slightly, then lift it back up. This works pelvic stabilizers that stop your trunk from tipping and dragging the knee in.
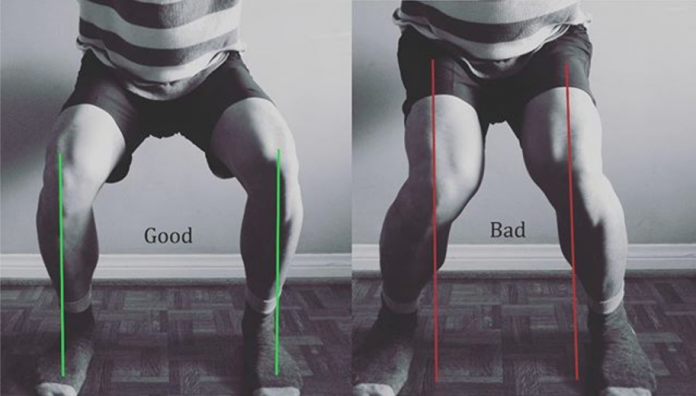
3. Integration: Connect Strength Into Movement
Strong muscles are only useful if they work in real-life motions. This step teaches your body to keep alignment during everyday patterns like bending, lunging, or lifting.
- Single-leg RDL → Balance on one leg, hinge forward at the hip, and reach ahead. This develops balance, hamstring strength, and trunk control, making the knee track straight instead of wobbling.
- Lateral lunges → Step to the side and bend into the hip. The move reinforces knee-over-toe tracking and builds power in the glutes.
- Squats and deadlifts with form focus → Use lighter weight at first. Train in front of a mirror or record yourself to check alignment. Biofeedback helps correct habits before they stick.
4. Plyometrics: Level Up for Athletes
If you play sports, you need to trust your landings and cuts. Plyometrics put your new control to the test.
- Drop jumps → Step off a low box, land softly with knees stacked over feet. This conditions your joints for absorbing force safely.
- Landing drills → Practice controlled landings from jumps, keeping hips back and knees aligned. It retrains your nervous system to handle explosive movement without collapsing.
Biofeedback: See What You’re Doing
Awareness is everything.
- Use a mirror or slow-motion video to spot inward drift.
- Place a mini-band around your knees during squats to give instant feedback if the band snaps inward, you’ll know you’re collapsing.
👉 For more on how hip and core control influence knee mechanics, check out our Sciatica + Uneven Hips blogs.
Lifestyle & Ergonomics for Knee Health
Strong knees aren’t built in the gym alone they’re shaped by how you sit, stand, and move all day. If your daily habits are off, even the best rehab plan won’t stick. Here’s how to keep the wins rolling:
Ergonomics That Don’t Suck
Slouched at your desk? Knees tucked under your chair? That setup is low-key wrecking your alignment. Ensure your desk setup promotes good posture; your screen should be at eye level to prevent slouching. Good ergonomics(designing your surroundings to fit your body’s needs) mean: hips and knees at 90°, feet planted flat, and your screen at eye level. Think of it as stacking your body so it doesn’t crumble over time.
Footwear & Orthotics: Your Base Layer
Shoes are the first line of defense. Worn-down soles or flat sneakers let your arches collapse, which pulls the knees inward. Solid footwear with arch support changes everything. For stubborn flat feet, custom orthotics keep your base locked in more stability, less strain.
Effective Warm-Up Routines
Cold muscles = sloppy movement. Quick warmup routines with ankle mobility drills, hip openers, and glute activations prep your body for action. It’s not extra work; it’s protection. Two minutes now saves you months of pain later.
Break the Sit Trap
Hours of sitting switch off the glutes and tighten hips. That combo is basically an invite for knees to cave in. Every hour, stand up, stretch, or crank out 10 bodyweight squats. Movement breaks keep your system online and your alignment sharp.
Daily habits either keep your knees tracking clean or slowly drag them out of line. Stack your environment and routines in your favor, and you’ll make the fixes to knee valgus last for the long run.
Prevention & Long-Term Management
Fixing inward collapse is great. Keeping it gone forever? That’s the real flex. Here’s how you lock it in for the long game:
Core Stability = Command Center
An unstable core makes everything below it unstable. Strong torso stability keeps your trunk stacked, pelvis steady, and knees tracking clean. Think planks, side planks, anti-rotation holds simple moves that keep the whole chain locked in.
Glute Strength = Built-In Braces
Your glutes are like armor. When they’re strong, the hips don’t wobble and the knees don’t cave. Hip thrusts, single-leg bridges, and step-ups keep them fired up. Skip this, and every squat or sprint falls apart.
Mobility Training = Freedom to Move
Tight ankles and stiff hips force your body to cheat. That cheat = collapse. Daily mobility training ankle dorsiflexion drills, 90/90 hip work, foam rolling gives your joints the range they need so your muscles don’t burn out.
Maintenance Routines = Stay Ready
Progress fades fast if you ghost the basics. A few minutes of maintenance routines (glute activation, mobility flows, core resets) 2–3 times a week is all it takes. Desk workers need it to fight stiffness, athletes need it to stay bulletproof.
Check out our Atlas prevention services for programs that make staying consistent way easier.
⚡The fix is just the start. The win comes from keeping your body strong, mobile, and switched on so knee collapse never sneaks back.
When to See a Professional
Corrective drills and daily changes help, yet sometimes knee valgus needs pro-level care. Leaving it alone only speeds up wear, so here’s when to bring in experts:
When to Call for Backup
- Physiotherapy → If you’ve been consistent for months with no change in knee valgus, physiotherapy is the next step. A therapist can run a detailed screen, target weak links, and create a progression that actually sticks.
- Chiropractic → Misalignments in the pelvis or spine often fuel the collapse. Chiropractic care paired with rehab brings your system back in line, helping hips and knees track correctly.
- Regenerative therapy → When conservative care fails, advanced options step in. Two big ones:
- Platelet-Rich Plasma (PRP) → A blood draw is spun down, growth factors are concentrated, then returned through targeted injections to calm inflammation and repair tissue.
- Stem Cell Therapy → Stem cells from your body are used to repair cartilage or ligaments, slowing joint damage and extending knee health.
Red Flags That Demand a Consult
- Mechanical axis deviation greater than 15°
The “mechanical axis” is the straight line that should ideally run from your hip → knee → ankle. In healthy alignment, that line passes close to the knee center. When the angle drifts more than 15° outward, it means the collapse is no longer just a movement quirk it’s a structural deformity. At this point, the uneven load on cartilage and ligaments is too great for exercises alone to fix.
- Failure of 6 months of conservative care, especially without progress from physiotherapy
Conservative care = exercise, mobility training, posture fixes, and physiotherapy. If you’ve been consistent for six months and knee valgus still looks the same (or worse), that’s a sign your system isn’t responding. This often means there are deeper issues, for example: severe hip weakness, joint degeneration, or bone remodeling, that need medical-level intervention instead of just home rehab.
- Progressive joint degeneration seen on imaging or physical exam
Suppose an X-ray, MRI, or even a hands-on test from a clinician shows thinning cartilage, joint space narrowing, or worsening instability. In that case, it means the collapse has already started damaging the joint. This is “progressive degeneration” basically your knee is wearing down faster than it can repair itself. Without pro-level care (sometimes including regenerative therapy or surgery), it usually continues to worsen.
At this stage, you need a professional plan that may combine advanced rehab with regenerative therapy or even surgery if the collapse is severe.
How Atlas Spine Clinic Can Help
At Atlas Spine Clinic, we know how frustrating inward knee collapse can be. It slows your workouts, messes with your stride, and chips away at confidence. That’s why our team blends chiropractic care, physiotherapy, and structured rehab programs to fix the root causes instead of just patching symptoms.
Here’s what sets us apart:
- Expertise that clicks → Our clinicians don’t just hand you generic exercises. They design strategies around your body, from hip strength to ankle mobility, so your results last.
- Real testimonials, real progress → From athletes getting back on the field to desk workers ditching chronic knee pain, our track record proves the system works.
- Complete approach → Hands-on treatment plus guided rehab = faster recovery and less chance of relapse.
Your journey doesn’t have to be trial and error. Book today and let’s build a plan to keep your knees strong for the long term.
📞 Call us at (647) 794-6868 or
🖥️ fill out our online form to book an appointment or learn more about our services.
FAQs
Q1. Can you fix knee valgus without surgery?
– Yes. Most people can fix knee valgus through physiotherapy, glute strengthening, ankle mobility drills, and motor control retraining. Surgery is only considered for severe structural cases.
Q2. Is adult correction possible?
– Absolutely. Adult correction just takes longer than in children, since bones are fully developed. With consistent rehab programs and lifestyle changes, alignment and function can still improve.
Q3. Does knee collapse during squats always mean valgus?
– Not always, but squat knee collapse is a common sign. Sometimes it comes from fatigue or poor motor control. If it happens regularly, it’s usually related to weak hips or flat feet feeding into the inward drift.
Q4. How does valgus alignment raise ACL risk?
– An inward collapse puts rotational force on the knee joint, increasing ACL risk. This is especially dangerous for athletes in cutting, pivoting, or jumping sports. Studies confirm valgus loading is one of the top predictors of ACL injuries.
Q5. How long does it take to see results?
– Progress depends on consistency. Some people see change in 6–8 weeks of focused training, while full correction often takes several months. The key is sticking to glute and core work, plus retraining your movement patterns.